Hi all,
I’m about analyzing if an old existing non-FHIR medication workflow can be replaced by a FHIR Medication workflow in compliance with all legal medication safety regulations. I already checked all the medication resources and I got that there are a lot’s of steps which can be replaced.
But now I’ve a few questions:
-
Is there a resource for barcode scans (for example for the scan of the barcode of a medicationplan)?
-
If a patient comes to hospital and brings all his private medicaments with him, these medicaments should be replaced by internal hospital medicaments. Which FHIR resource / workflow should be used in this case?
-
As I understand the FHIR medication workflow and resources there’s always only one medicament listed in one resource. So if I want a list of all medicaments the patient takes, I have to collect them into a bundle to get a whole medication plan? From this question results the next one:
-
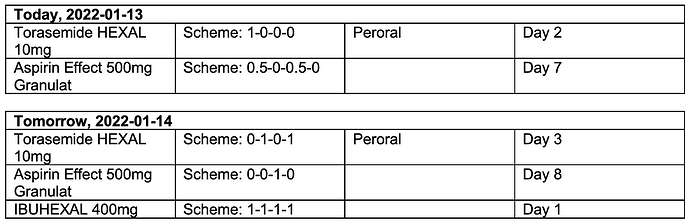
Is it possible to display a time beam like a calendar to see per day which medicaments the patient takes at which day? Like in this quick example: If I click to the next day in a time beam I would like to get the second list for the next day.
- If a product wants to go international and so can’t use the implementation guide of its country, how is the interoperability granted if there are different medication profiles?
Sorry for this amount of questions, but these are two difficult and important issues: FHIR and medication… ![]()
Thanks in advance and regards.
Lisa